Study: Ten-year Retrospective Study on the Efficacy of a Manual Physical Therapy to Treat Female Infertility Alternative Therapies in Health and Medicine – 2015
Description: This landmark study examined the results treating 1,392 infertile women treated with the Clear Passage Approach (CPA) at all of our clinics, between 2002 and 2011. The study compares success rates of CPA to traditional medical treatments (surgeries and pharmaceuticals).
Results: Success rates with CPA therapy rivaled or exceeded medical success rates in some common causes of female infertility: Blocked fallopian tubes, endometriosis, PCOS (often accompanied with failure to ovulate), and advanced age, measured by high FSH hormone levels. In some areas (such as endometriosis) the results were comparable to surgery, but avoided surgical risks. In some cases such as Primary Ovarian Failure (POF) we did not do well at all. We present those numbers, as well.
Some side-effects of therapy were transient, such as temporary soreness after therapy. Lasting side-effects such as increased desire, lubrication and orgasm, and decreased or eliminated intercourse or menstrual pain are presented separately, in the Pelvic Pain section of this website page, along with endometriosis pain and dysfunction.
While the great majority of our successes were natural, the therapy also increased in vitro fertilization (IVF) pregnancy rates significantly in all age groups, when performed before embryo transfer, with fairly dramatic success in women who were nearing the end of their reproductive age. For example, rates in women over 40 were roughly three to five times the norm.
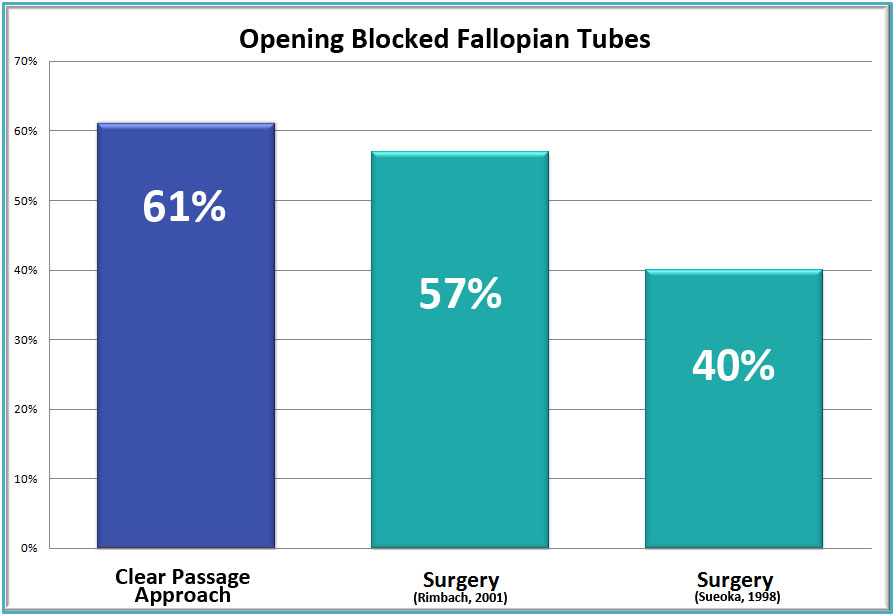
Opening Blocked Fallopian Tubes
Results:
The therapy opened totally blocked fallopian tubes in:
69% of women with no prior tubal surgery (124/180)
35% of women with prior surgery to their tubes (19/55)
61% of women overall (143/235)
60% rate opening blocked fallopian tubes in women with endometriosis (40/67)
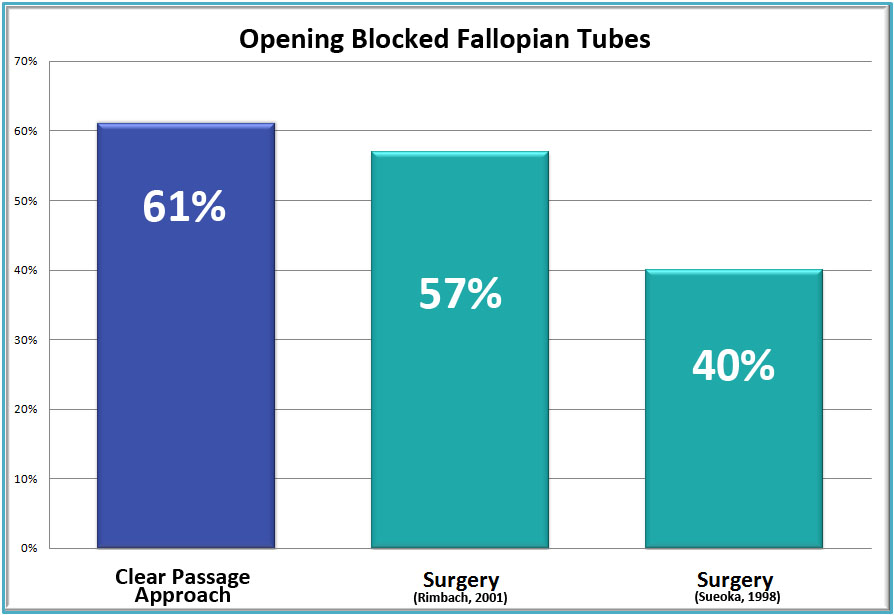
In largest published study of its type, CPA therapy opened totally blocked fallopian tubes in 61% of (143/235) women diagnosed with total tubal occlusion (both tubes blocked) before therapy. Of interest, this rate matched the percentage cited in Contemporary Ob-Gyn[i] in 2008, which showed a 61% success rate for CPA opening tubes in (17/28) women in a pilot study conducted seven years earlier.
Success rates in the larger study were 69% for (124/180) for women who had not undergone prior tubal surgery and 35% for (19/55) women who had undergone a prior tubal surgery. The lower rate was surmised to be caused by post-surgical scarring on the delicate fallopian tubes.
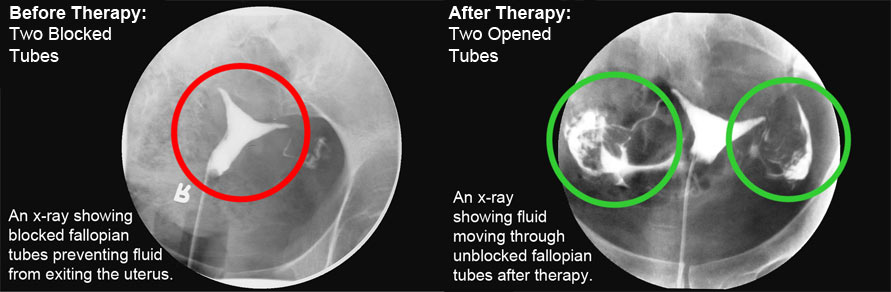
Pre- and post-therapy results were measured by dye tests, surgery or natural pregnancy, which can only occur to open tubes.
Clearing Hydrosalpinx
RESULTS: 45% cleared of hydrosalpinx (47/105)
Per the 10-year study (2015), the CPA opened tubes in 45% (47/105) of women with hydrosalpinx (liquid-filled tubes), a very challenging group. Reproductive physicians often remove tubes with hydrosalpinx, feeling they will never function, yet the therapy returned fertility for many of these women. Interestingly, this rate confirmed the rate of their very first pilot study treating women with hydrosalpinx, presented to the American Society for Reproductive Medicine (ASRM), and published as an abstract in 2006, when the therapy cleared tubes in 50% of women with hydrosalpinx.
Pregnancy Rates For Women With Cleared Tubes
RESULTS: 57% (81/143) pregnancy rates after therapy
- 80 natural pregnancies; 1 via IVF
- Several women experienced additional (second or third) natural pregnancies after treatment suggesting the results of therapy can last for many years.
In the large 10-year study, pregnancy rates for women whose tubes were opened by the therapy were 57% (81/143) after therapy (vs. 22% – 34% after surgery).
Notes:
- Location of the blockage did not influence clearance rates;
- While surgery can often open tubes that are proximally blocked (near the uterus), surgically opened fallopian tubes tend to close within six months after surgery because of post-surgical scarring. In the largest study ever conducted on follow-up after tubal surgery, a repeat HSG dye test six months after opening tubes by surgery showed a total re-occlusion rate of 81% (35/43), six months after surgery viii.
Endometriosis – Overview
Endometriosis is a complex condition that contains both mechanical and hormonal elements. In this condition, endometrial tissue that is normally found in the lining of the uterus, and that should be expelled with every menstrual period, is found in the interstitial spaces of the body – between organs, muscles, nerves and bones. When a woman has a period, these endometrial implants swell, pulling on the adhesions that frequently form between the implants and the structure on which they reside. The main concerns for women with endometriosis are
- infertility
- moderate to severe period pain
- moderate to severe pain with intercourse
- decreases sexual function (e.g., desire, lubrication, orgasm)
CPA therapy has been studied in all of these areas. In all cases, the therapy is designed to decrease the cross-linking, the tiny but powerful white attachments shown in the drawing in the URL covering endometriosis. Below is data on infertility reversal for women we treated with endometriosis. Results of the reversing pain and sexual dysfunction are given later on this page.
Endometriosis Related Infertility
RESULTS: 43% (128/299) pregnancy rate
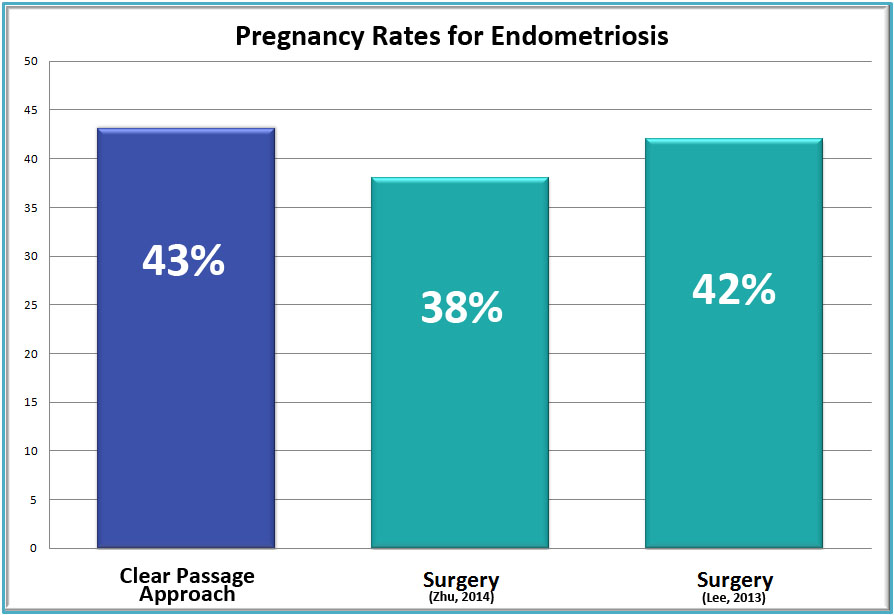
In the 10-year study, the therapy yielded pregnancy rates of 43%, which is comparable to the 38%[i] to 42%[ii] success rates of surgeries cited in the study. Therapy avoids the risk and cost of surgery, including anesthesia, inadvertent enterotomy (cutting through or into nearby structures mistakenly), and post-surgical adhesions.
Of the 56 patients with follow-up who underwent IVF post-CPA treatment, the clinical pregnancy rate after transfer was 55.4% (31/56), which is 1.3 times that of the national average of 40.3% for IVF transfer alone in women with endometriosis.
PCOS – Infertility
RESULTS: 54% (15/28) pregnancy rate, 14 natural pregnancies; 1 pregnancy by IVF
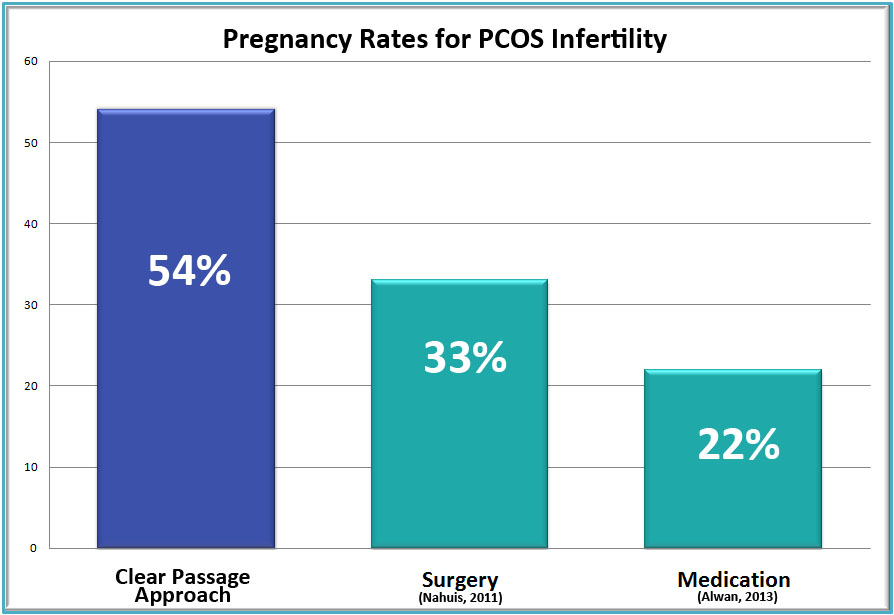
In a subset of women experiencing infertility due to polycystic ovarian syndrome (PCOS), the non-surgical physical therapy yielded a 54% (15/28) success rate. While this subset is not large, it is promising. The results compare well with the 22%[i] to 33%[ii] success rates for medications and surgery, which generally consists of ovarian drilling (cutting holes through the tissues surrounding the ovary, and then into the ovary itself) and ovarian wedging (cutting a wedge-shaped piece out of the ovary.)
Comparison to medications and surgery: According to the study published in 2015: Options for standard medical treatment of PCOS include medications—clomiphene citrate, metformin, or combinations thereof —and surgical interventions to induce ovulation. The rates of pregnancy in patients treated using the CPA were directly compared with success rates for various interventions reported in the literature. The CPA demonstrated significantly higher rates of pregnancy when compared with metformin alone. CPA treatment presented no significant differences in rates of pregnancy when compared with clomiphene citrate or the surgical interventions of ovarian wedging or drilling.
High FSH – Hormone Related Infertility
RESULTS: 38% pregnancy rate in our initial pilot, 2009 study (6/16)
(All pregnancies were natural in the pilot study)
39% pregnancy rate in our large, 2015 study (48/122)
43 pregnancies by natural conception; 5 pregnancies via IVF
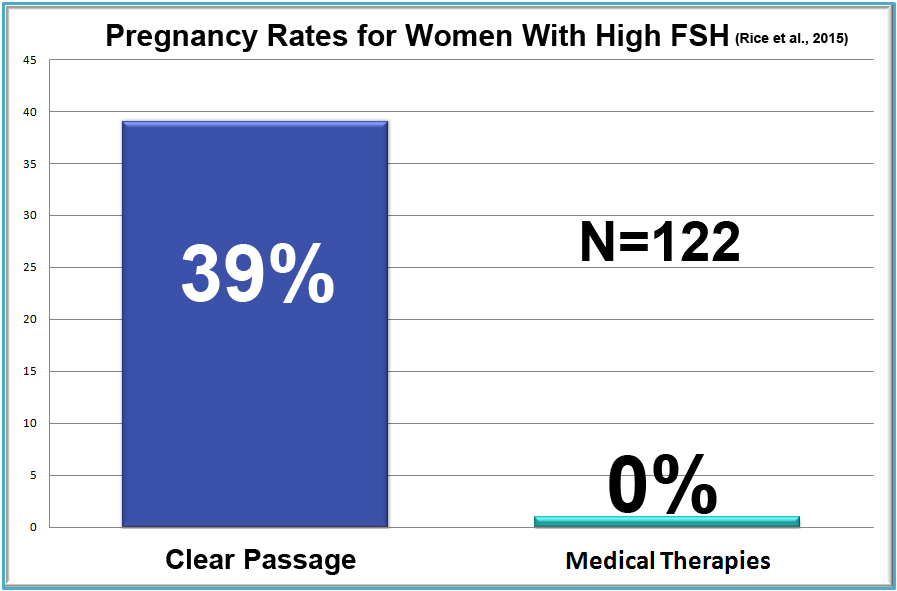
In a total surprise, CPA therapy improved hormonal fertility for women with high FSH (follicle stimulating hormone) levels. FSH levels (measured on Day 2 through 5 of a woman’s cycle, typically rise as a woman approaches menopause. When FSH levels are above 10 mIU/mL, most reproductive physicians consider the patient subfertile or infertile. In fact, many reproductive endocrinologists will not consider performing IVF (in vitro fertilization) on a woman with FSH levels at 10 or above. Because no standard medical treatment has been shown to improve fertility in women with high FSH, no comparison could be made between the therapy and standard medical treatments.
In the 10-year study, CPA therapy treated 122 women who were diagnosed subfertile or infertile, due to FSH levels above 10. The therapy, improved FSH levels or yielded pregnancy in 49% of the women, and 39% (48/122) of them became pregnant following therapy; 43 or the pregnancies were natural, and five were by IVF.
Pre-IVF Therapy
RESULTS: 56% pregnancy rate (82/146) for women who had CPA therapy before embryo transfer. This is 1.5 times higher than that of the national average of 37%. (SART 2010 data)
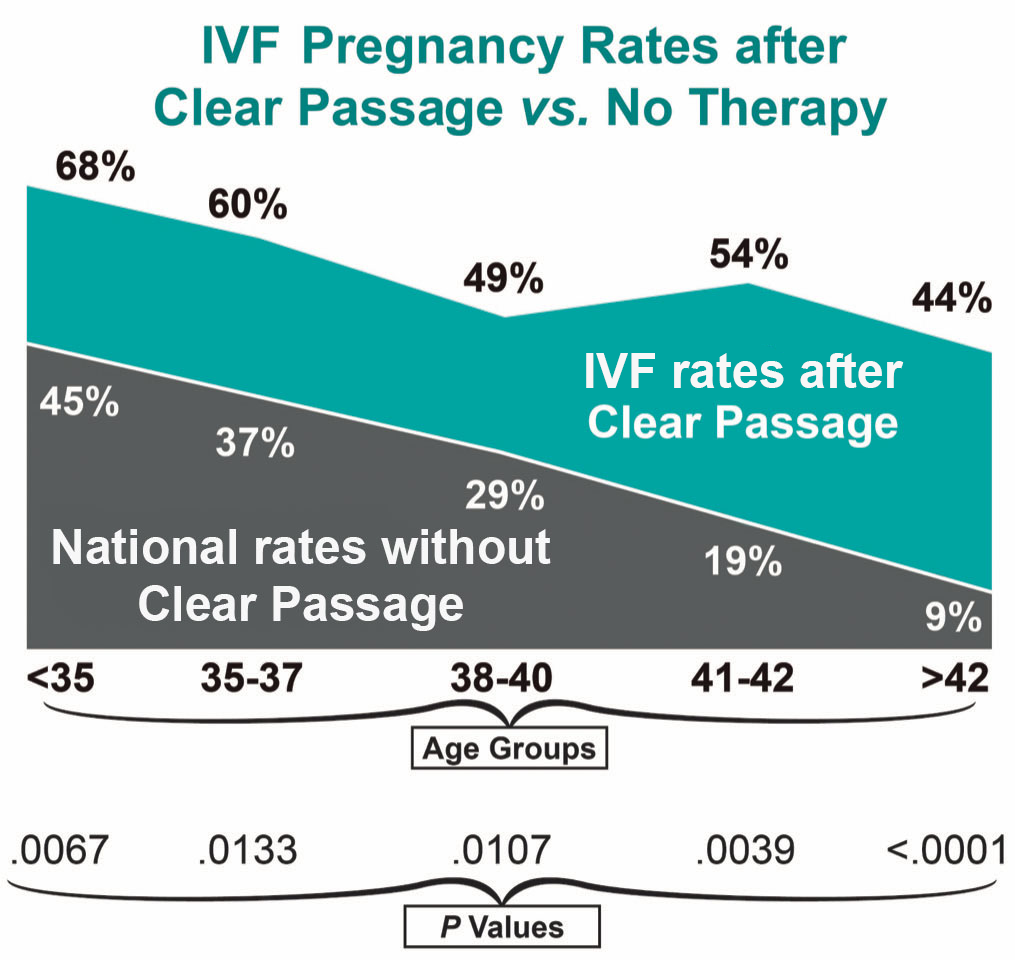
* P-value is a statistical term used to measure results. The P-values above are considered excellent, providing validity to the results.
In these cases, the therapy focused on decreasing adhesions and collagen crosslinking in four areas:
- The uterus and cervix;
- The ovaries and fallopian tubes;
- The dura, the collagenous covering of the spinal cord which runs from the coccyx (tailbone) in the pelvis to the cranial base (at the occiput), then into the cranium;
- At the pituitary and hypothalamus, via the dura and the osseous structures (bones) that comprise the cranium, and encase the pituitary gland.
In these cases, the therapy focused on decreasing adhesions and collagen crosslinking in four areas:
- The uterus and cervix;
- The ovaries and fallopian tubes;
- The dura, the collagenous covering of the spinal cord which runs from the coccyx (tailbone) in the pelvis to the cranial base (at the occiput), then into the cranium;
- At the pituitary and hypothalamus, via the dura and the osseous structures (bones) that comprise the cranium, and encase the pituitary gland.
Primary Ovarian Failure – POF
RESULTS: 20% (1/5 patients) pregnancy rate in patients with POF via natural conception
While it is difficult to gather meaningful data from a subset of only five patients, initial results indicate that we do not offer any meaningful improvement for women diagnosed with Primary Ovarian Failure (POF). Nevertheless, we do have good success for women with advanced reproductive age. We are glad to speak with you about your specific case and needs.
Related Content:
- Women’s Infertility Published Success Rates
- Hope After Seven Years of Infertility
- Meet the Clear Passage ‘Miracle Babies’!
- Overcoming Infertility: Three Friends Share Their Success Story with “Fertility Massage”
- Patient Video: Two Miracle Babies and a New Body
- Three Friends Overcome Years of Infertility With ‘Massage’ When Recently Investigated Hands-On Therapy Succeeds After Medical Science Fails
If you’d like a free consult, please take 20 minutes and fill out this form and we can determine if therapy would be a good fit for you.