Medscape General Medicine – 2004
Increasing Orgasm and Decreasing Dyspareunia
(Painful Intercourse) by a Manual Physical Therapy Technique
The first major study on our work treating pelvic pain and sexual dysfunction was published in 2004. We were honored that this study (data above) was published in Medscape General Medicine, owned by WebMD. At the time, it was the largest medical journal in the world, accessible to physicians in 237 countries. The editor was George Lundberg, MD, who had been editor of the Journal of the American Medical Association for the prior 17 years.
This study assessed the improvements of intercourse pain and overall sexual function in women with a history of chronic pelvic pain. In this population, 96% of patients reported a decrease in intercourse pain after CPA treatment and 91% reported an increase in overall sexual function.
Endometriosis Pain – Overview
Endometriosis is a complex condition that contains both mechanical and hormonal elements. In this condition, endometrial tissue that is normally found in the lining of the uterus, and that should be expelled with every menstrual period, is found in the interstitial spaces of the body – between organs, muscles, nerves and bones. When a woman has a period, these endometrial implants swell, pulling on the adhesions that frequently form between the implants and the structure on which they reside. Besides infertility, the main concerns for women with endometriosis are
- moderate to severe period pain
- moderate to severe pain with intercourse
- decreases sexual function (e.g., desire, lubrication, orgasm)
CPA therapy has been studied in all of these areas. In all cases, the therapy is designed to decrease the cross-linking, the tiny but powerful white attachments shown in the drawing on the URL covering endometriosis. Below is data on reversing pain and sexual dysfunction for women we treated with endometriosis.
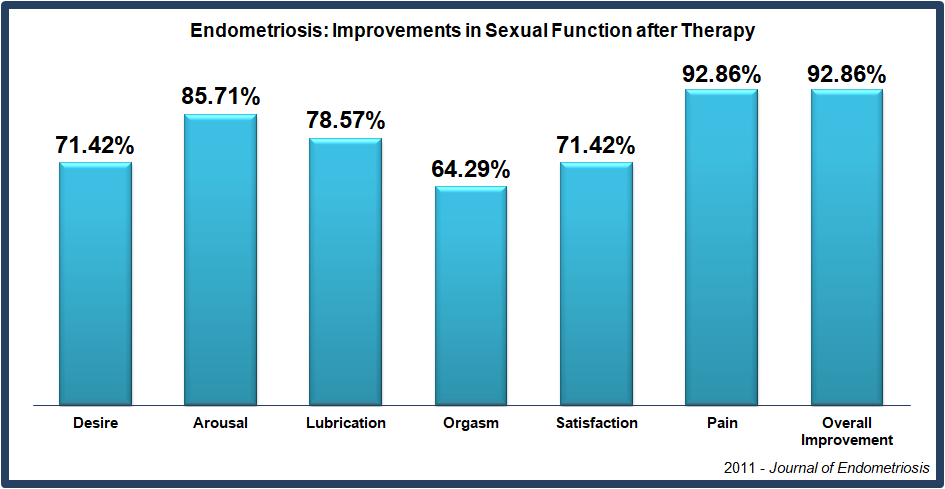
Pelvic Pain and Sexual Function Improvements – Endometriosis
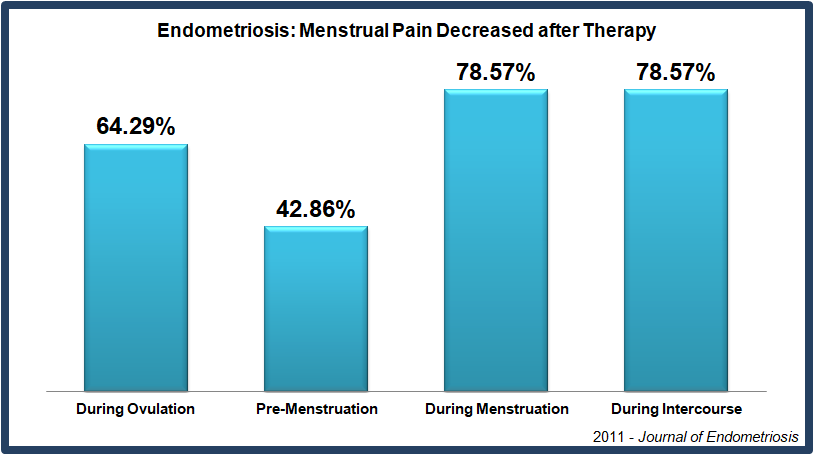
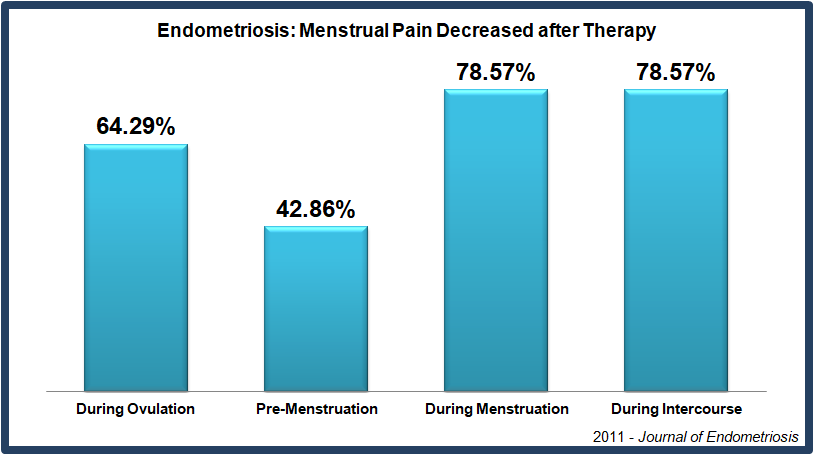
A 2011 study in the Journal of Endometriosis and Pelvic Pain Disorders reported on the effects of CPA on women who had endometriosis, menstrual and intercourse pain, and sexual problems. This two-part study was retrospective for women with sexual pain and dysfunction, and prospective for a different group of women, who had menstrual and intercourse pain. A follow-up study published in the same journal (2014) reported the effects of the therapy lasted over a year – which is the same time-frame used to test the effectiveness of endometriosis surgery.
While these studies were relatively small, the results were substantial enough to be considered valid (called statistically significant) by the biostatistician. In the retrospective analysis CPA therapy showed statistically significant improvements (P=.001) for every domain of sexual function listed above, including dyspareunia [intercourse pain] (P>.001), measured by the Female Sexual Function Index test. In the prospective analysis, CPA therapy showed statistically significant improvements in pain levels during the menstrual cycle (P>.014), with dysmenorrhea [menstrual pain] (P=.008) and with dyspareunia [intercourse pain] (P=.001), using the Mankoski Pain Scale.
Endometriosis: Menstrual pain, intercourse pain, sexual function
Journal of Endometriosis – 2011
Decreasing Dyspareunia and Dysmenorrhea in Women with Endometriosis via a Manual Physical Therapy: Results from Two Independent Studies
This study assessed pain in women with endometriosis after treatment with the Wurn Technique. 61% of women in this study reported a reduction in menstrual pain and 80% reported a decrease in intercourse pain. Additionally, patients reported improvements in female sexual function, with 93% reporting improvements in overall sexual function.
We tracked pain relief for one year, to compare with studies on surgical success rates. Results show success rates with this therapy are comparable to surgery (no better, and no worse), but without surgical risks, including of post-surgical adhesions.
Studies were published in the Journal of Endometriosis, 2011 (initial study) and 2014 (one year follow-up)
Statistical study data:
Female Sexual Function Index (FSFI) Full Scale score showed overall statistically significant improvements (P=.001) for all domains of sexual function, including dyspareunia [intercourse pain] at (P>.001) in the retrospective analyses. Measured via the Mankoski Pain Scale, statistically significant improvements were noted in menstrual cycle (P>.014), dysmenorrhea (P=.008) and dyspareunia (P=.001) in the prospective analyses.
If you’d like a free consult, please take 20 minutes and fill out this form and we can determine if therapy would be a good fit for you.