Table of Contents
Clear Passage®️ is a world leader with over three decades of experience in the non-surgical opening of fallopian tubes diagnosed with hydrosalpinx (swollen tubes). Once opened by us, formerly swollen tubes drain the liquid within them, and fertility returns for many women. The therapy, which can feel like a slow and deep site-specific massage, has been shown in numerous peer-reviewed studies to decrease the internal scars called adhesions that are a primary cause of hydrosalpinx.
Adhesions can form anywhere in the tube after a surgery, injury, infection, or endometriosis. They can act like a glue in the female reproductive tract, blocking fallopian tubes or narrowing the ends of the tube to near or full closure, creating or augmenting a hydrosalpinx. Adhesions and crosslinks can spread to bind or squeeze any of a woman’s reproductive structures like internal straitjackets.
Over 1,000 babies have been born to women diagnosed infertile after treatment at Clear Passage®️ clinics. The therapy has been shown to open totally blocked fallopian tubes and return function to tubes with hydrosalpinx for some women. Once freed of the distal adhesions, tubes tend to clear as the liquid drains away. When this occurs, function and fertility have returned for many women. Some women have reported two or more natural pregnancies and births after we opened their formerly swollen tubes.
Click here to view our published infertility success rates and video testimonials. Complete the online Request Consultation form to share your medical history so we can intelligently converse with you about your case (no charge.)
Causes and Frequency of Hydrosalpinx
Hydrosalpinx is a condition that occurs when a fallopian tube is totally or partially blocked at the distal end of the tube, near the ovary. Swelling occurs due to fluid buildup that interrupts the natural passage of egg and sperm through the tube. Hydrosalpinx is just one aspect of tubal disease which may include tubal occlusion (totally blocked fallopian tube).
Tubal disease accounts for 20% to 30% of all female infertility. The incidence of hydrosalpinx (swollen tube) in infertile women is between 10% and 13% when diagnosed by ultrasound but may increase to 30% when diagnosed by hysterosalpingogram or laparoscopic surgery – generally considered more accurate tests due to the increased quality of the images.
A Deeper Look at Swollen Tubes
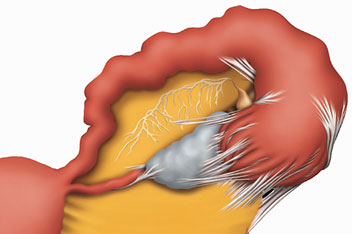
In hydrosalpinx, the tube becomes distended, giving the tube a characteristic sausage-like shape as shown here. The fluid buildup may occur in one or both tubes. A tube with a hydrosalpinx is considered beyond repair by many physicians who feel it will never support a pregnancy or recommend a surgical procedure. We found this not to be true when several patients who came to us with hydrosalpinx had natural full-term pregnancies after we treated them with no surgical procedure required.
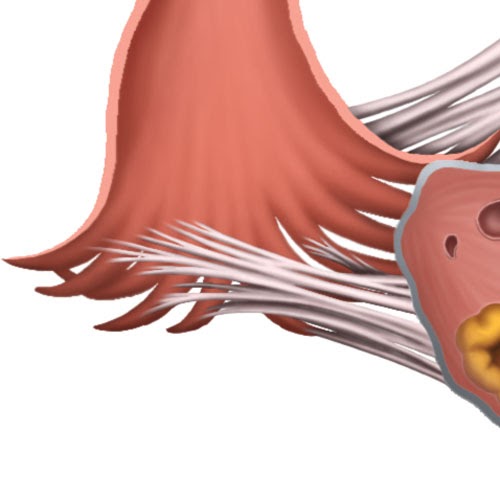
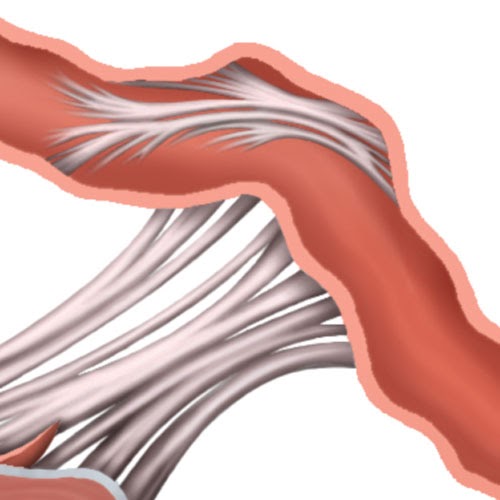
Swollen tubes are usually partly or fully blocked by adhesions that form at the distal end (near the ovary). This blockage is generally attributed to adhesions, internal scars that form as the first step in healing from an infection such as PID (pelvic inflammatory disease), surgery or endometriosis. Acting like a glue in the reproductive tract, adhesions are comprised of tiny but powerful collagen fibers that bind to each other in a chaotic pattern to form an internal scar. On a microscopic scale, these collagen fibers bind together via crosslinks that bind them. We believe that our work tends to disrupt or dissolve the crosslinks that have formed, allowing the structure to return to an earlier, more functional anatomy.
Fallopian tubes are the delicate organs that provide a pathway where life begins. Their interior can be compared to a slow-moving river that helps transport a woman’s egg down to meet a single sperm – to create a new life to implant and grow within the uterus. With a hydrosalpinx, there is a blockage or narrowing at one end of the river. The tube swells to create a large lake within the tube. Without the flow of the river, the sperm and egg can become lost within the lake, so they never meet.
Even if they meet and fertilization occurs, the risk is high that the fertilized egg will become ‘lost’ in the lake of fluid within the tube, resulting in an ectopic pregnancy. When this occurs, the embryo never leaves the tube. It begins to grow there and must be destroyed by an injection of methotrexate. If the injection is delayed too long, a surgeon will remove the tube altogether to save the mother’s life. In either case, the pregnancy will be lost.
Our History Treating Hydrosalpinx
Since we began investigating in 1984, the founders of Clear Passage® focused all our efforts at decreasing been adhesions. We were initially surprised when the therapy began opening totally blocked fallopian tubes. With a local gynecologist-surgeon, we began to investigate this phenomenon.
One of our first surprises was a woman who had two natural pregnancies and births after we treated her only tube – which was shown in diagnostic tests before therapy to be totally blocked and severely swollen with hydrosalpinx. When she had her first natural full-term pregnancy after therapy (she actually had a subsequent natural pregnancy, this time with twins), our curiosity was piqued. We started to investigate. Here is what we found:
After numerous natural pregnancies occurred in women who came to us with total bilateral occlusion (both tubes completely blocked), we began to document pregnancies and births in women who had only one tube, and that tube was swollen with a hydrosalpinx. We presented our initial data on infertility reversals in this population at the annual meeting of the American Society for Reproductive Medicine in 2004, which published our work in their professional journal Fertility and Sterility that year.
Additional value
Over time, we have found that therapy to address the adhesions that cause hydrosalpinx has additional value. After adhesions form, they can remain in the body for a lifetime. When they form at the distal end of the tube (near the ovary), they can cause swelling of the tube – a hydrosalpinx. From there, adhesions can spread into any part of the reproductive tract or pelvis, including the bladder, rectum, bowel, tailbone or low back. They can squeeze any of these structures or attach them to others, further decreasing fertility and sometimes causing pain.
Adhesions can form on the outer walls of the uterus, squeezing it and causing spasm, decreasing the chance for implantation. Adhesive crosslinking can also form on the inner walls, covering parts or all of the surface designed to accept a fertilized egg, which we feel can contribute to miscarriage. As we treat, we address the entire reproductive tract within the pelvis. Over the five days of therapy, we will move up to body into tissues that surround the spinal cord (the dura). We progress into the collagenous offshoots of the dura which surround the pituitary gland – the master gland of female reproduction. In short, our therapy works to decrease adhesions that create or support a hydrosalpinx in many of the women we treat with this condition. At the same time, we work to decrease adhesions throughout the reproductive tract and into the brain, to increase a woman’s chance for pregnancy – whether natural or assisted by IVF.
Symptoms of Hydrosalpinx
It is common for women who have a hydrosalpinx to not experience any symptoms. Often the presence of a hydrosalpinx is only discovered upon failure to conceive. Here are some symptoms that can be present:
- Abdominal pain in the lower abdomen
- Pelvic pain
- Abnormal discharge
- Ectopic pregnancy
- Abnormal vaginal bleeding
If you are experiencing any of these symptoms along with infertility, it is quite possible you have a hydrosalpinx.
Treatments for Hydrosalpinx
Medical Treatments
We know of no commonly accepted medical treatment to reverse hydrosalpinx. Most reproductive physicians suggest removing the affected tube(s) and proceeding directly to in vitro fertilization (IVF).
Clear Passage®️ Therapies
Clear Passage®️ is a manual (hands-on) physical therapy shown in numerous medical journal studies to decrease or eliminate adhesions throughout the reproductive tract. Treatment consists of 20 hours of manual therapy, generally given at four hours a day (2 in the morning, 2 after lunch) over five days (e.g., Monday through Friday.) Most people travel for therapy arriving and leaving on the weekend.
Therapy is performed in a private treatment room. It can sometimes feel very light; at other times, it can feel like a quite deep, site-specific massage. We invite patients to bring a partner, relative or friend is she wishes, as she will have free time to explore the local area when not in therapy.
The focus of the therapy is to detach the tiny but powerful collagen fibers that comprise adhesions from each other by dissolving the molecular-chemical bond that attaches them. In doing so, the adhesions tend to unravel and dissipate, much like pulling out the run in a three-dimensional sweater.
In published studies, the therapy has shown success and natural pregnancies after clearing adhesions associated with swollen tubes. When a hydrosalpinx clears during therapy, the liquid trapped within the tube flows out and the tube appears to return to its normal structure and function. The result has been one or more pregnancies for many women.
No medical techniques have 100% success rate. In published studies, we appear to clear swollen tubes (hydrosalpinx) about 50% of the time. Once cleared, the tubes appear to return to their prior state of function and ability to carry a pregnancy. If we are unable to open your swollen tube(s), your chances for a successful IVF performed within 15 months after therapy increase by roughly 50%, per published studies. Click to view our success rates.
Each IVF cycle is designed to help sperm and egg meet and then implant in the uterus. If the cycle is not successful, it must be repeated. Raw data from The U.S. Centers for Disease Control (CDC) show a 24.11% national success rate for Assisted Reproductive Techniques such as IVF in the U.S.A.
DRUGS
No medication, topical or internal medication or treated/herbal tampon has been shown to be effective for opening blocked fallopian tubes.
Published Success Rates
Clear Passage®️ Success Rates
View all Infertility Success Rates by clicking here
View a Timeline of Clear Passage®️ Published Studies at the bottom of this page
In our earliest pilot studies, Clear Passage®️ therapy opened tubes with hydrosalpinx at a rate of 50%. As we progressed into a 10-year study of 1392 infertile women we treated, the success rate clearing hydrosalpinx was 45% (47/105), with no further evidence of hydrosalpinx. The overall pregnancy rate for women whose tubes we opened was 57% (81/143). All of the women who conceived after we opened their swollen tubes did so naturally. These results are considered remarkable in a population that had zero chance of natural pregnancy before therapy.
Natural pregnancies
As shown above, over half of our patients whose tubes opened became pregnant; several have had more than one child by natural conception without the need for further therapy.
|
Clear Passage®️ Success Rates[1] |
|||
|
61% |
45-50% |
57% |
56% |
|
Opening Blocked Fallopian Tubes |
Clearing Hydrosalpinx |
CP Pregnancy after Opening |
IVF Pregnancies After CP Therapy |
IVF and Surgical Success Rates
IVF National Success Rates
Surgical removal of the swollen tube followed by in vitro fertilization (IVF) is often suggested for women who present with hydrosalpinx. Statistics are gathered and published annually by the U.S. Centers for Disease Control (CDC) which charts the success rates for the several hundred reproductive clinics and physicians that report their data. This data is generally reported for 2 to 3 years’ prior to allow researchers to gather and compile data on pregnancies and live births. Statistically, CDC shows a 24.11% pregnancy rate for all Assisted Reproductive Techniques in the USA, 99% of which are IVF. (CDC, 2018) However, it is becoming difficult to tally the exact rate as physicians have begun to offer “egg banking” in which cycles are started, eggs are extracted, then saved for future transfer. For a more complete explanation, visit out “Calculate My Odds” page.
Published Research – a Timeline of Published Studies
Clear Passage®️ is committed to scientific inquiry and verifiable fact. Successive studies examining our success opening blocked fallopian tubes were published in 2004, 2006, and 2008[ii],[iii],[iv] These included three abstracts (summaries) published in Fertility and Sterility (2006)iii, the professional journal of all US based reproductive physicians. A large study of 1392 infertile women we treated over a 10-year period was published in 2015[v].
Our studies are designed, conducted, authored and peer-reviewed by physicians, biostatisticians and independent researchers. They show that Clear Passage® has opened tubes with hydrosalpinx and had natural pregnancies with rates that rival more complex medical methods, and often leave the tubes intact and functional.
If you’d like a free consult, please take 20 minutes and fill out this form and we can determine if therapy would be a good fit for you.