We Treat Intercourse Pain Naturally, Without Surgery or Drugs
Patients often report profound changes after receiving our hands-on, non-surgical therapy for painful intercourse.
Our therapists decrease pain, increase sexual intercourse, and restore the pleasure of intimacy and intercourse for most of the women we treat for pain. In doing so, we enrich their lives and those of their partners. We are one of the only therapy groups to have treated a large enough population that we can report our results in peer-reviewed medical journals, available at the National Library of Medicine
Causes and Frequency of Dyspareunia (Intercourse Pain)
Sixty percent of women in the U.S. report pain with intercourse (also called dyspareunia) at some point in their lives. (Heim, 2001) Intercourse pain that recurs or worsens over time is called chronic dyspareunia, a condition that can disrupt a woman’s relationship with her partner and cause moderate to debilitating pain at a time when most women experience great pleasure.
For many women, the search for a cure becomes a frustrating and unproductive journey of referrals from one doctor to another (gynecologist, urologist, pain specialist). Adding to the frustration, many are told to consult a psychologist or psychiatrist because the pain “must be in your head.” But their pain persists because it actually occurs in the vagina, precisely where they feel it. As a result, we find that telling a patient that intercourse pain is “all in your head” is generally inaccurate and totally disempowering.
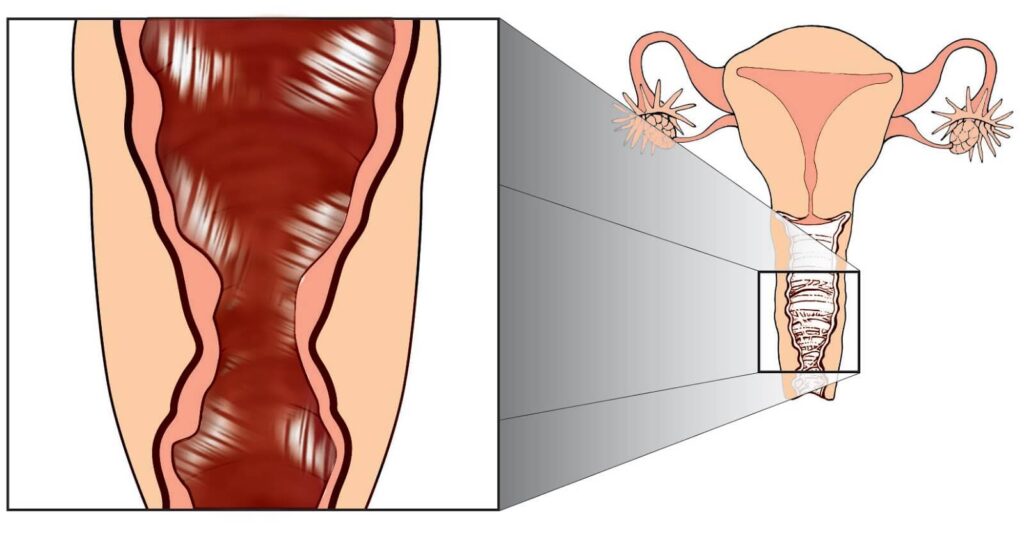
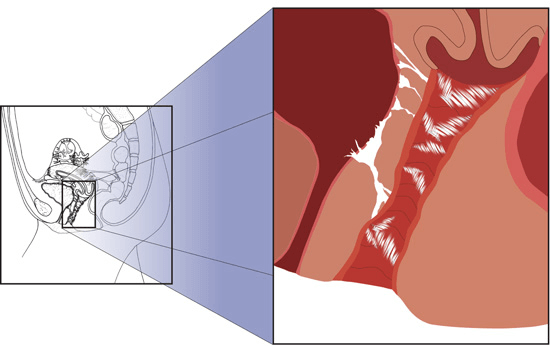
Pain at the Vaginal Entrance
When the body heals from an infection, trauma, or surgery, it forms tiny but powerful collagen cross-links–the building blocks of adhesions. These tiny internal scars act like straitjackets, attaching to the vaginal wall or entrance or other pain-sensitive structures. Robbed of their usual elasticity, the adhered tissues cause pain when a finger, penis, or other device enters instead of the pleasure that should come from intercourse.
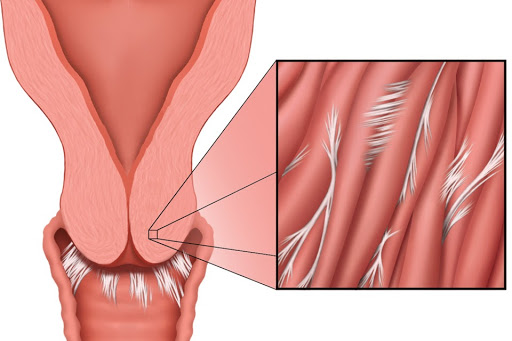
Pain With Deep Penetration
Tiny adhesions that form at the tailbone (coccyx) after a fall can pull that structure forward, causing pain when a woman’s partner hits that structure during deep penetration. Adhesions can also form between muscle cells deep within the cervix (stenosis of cervix), causing a similar deep pain during sexual intercourse.
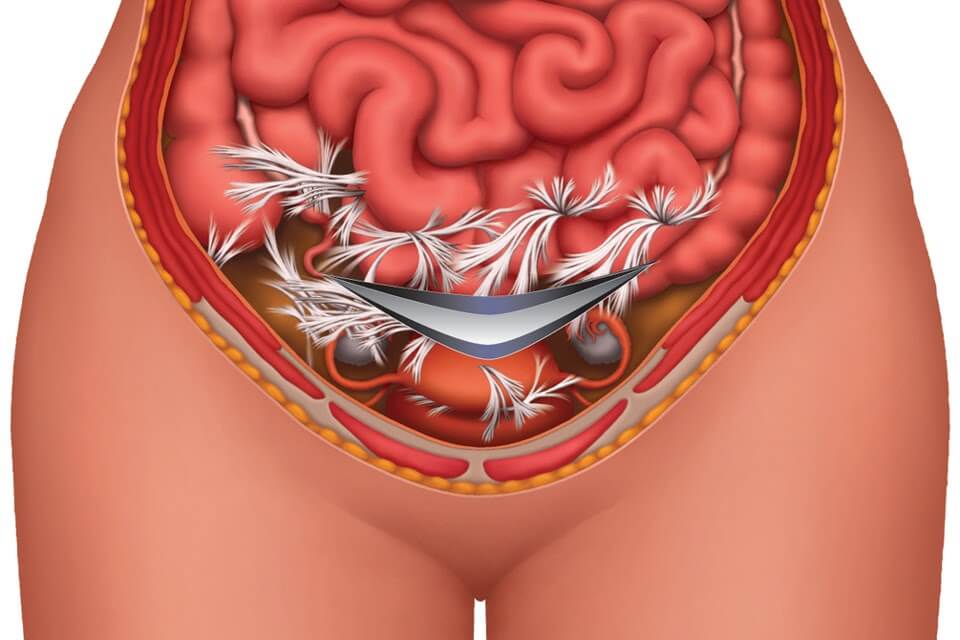
Adhesions form in response to any of the infections, inflammations, surgeries, or traumas to which the female reproductive tract is subjected. Conditions that cause these adhesions include:
- Endometriosis
- Physical or sexual abuse
- Intercourse when not fully lubricated
- Bladder or vaginal infection or inflammation
- Vaginismus (a spasm of the muscles around the opening of the vagina)
- Surgery (e.g. abortion, episiotomy, C-section, hysterectomy, female circumcision)
- Trauma to the tailbone, pelvis, or nearby structures (hip, low back, etc.) such as a fall or sports injury (e.g. a cheerleading, skating, horseback riding, or bicycle injury)
Treatment Options for Dyspareunia
Clear Passage®️ Treatment
In the hundreds of women we have treated for dyspareunia pain, we usually find that tiny adhesions, or internal scars, are the direct cause or significantly contribute to their pain. Physicians often overlook these small, sometimes microscopic structures for several reasons. Adhesions can be so small that they are often difficult or impossible to view, even using advanced medical imaging such as CT, MRI, ultrasound, or X-ray. In addition, adhesions are nearly impossible for doctors to treat when they form on or within the delicate tissues of the vagina.
Our therapists use their hands and a protocol of over 200 manual techniques to detach pelvic and vaginal adhesions, often reducing or eliminating dyspareunia pain permanently. We always work well within the patient’s tolerance level and the patient is always in control of the pressure we use at each moment during therapy. Most of our therapy is external, as we treat the legs, hips, and other structures that attach to the areas of pain. If we treat internally, we use a gloved hand and work slowly and gently. All therapy is performed with respect and dignity in a private treatment room, following established guidelines for draping and the presence of chaperones. The patient always has the choice to refuse internal therapy, although it is highly recommended for dyspareunia.
We direct therapy to the areas that are causing symptoms. For some women, pain may occur at first penetration as a sharp and specific pain in one or more locations at or near the opening of the vagina. Others experience pain with deep penetration. They generally describe a broader, deeper pain ̶ as if “… my partner is hitting something.” Some women experience pain in both areas.
Women who bring their partner along to therapy are able to test their progress during the week. This feedback can help us determine which areas are being relieved and which areas still need attention during upcoming treatment sessions.
Some women absorb repetitive traumas and stresses to the pelvis without experiencing symptoms or negative side effects. However, some women experience significant, long-lasting symptoms, as tiny but powerful adhesive fibers rob their bodies of the easy mobility and extensibility of normal tissues.
Bound by adhesions, they may also experience other symptoms, such as anorgasmia (inability or difficulty reaching orgasm) and decreased desire or lubrication. When we treat the vaginal tissues, these symptoms generally resolve or improve dramatically. Our work addresses all of these conditions, with positive results generally lasting years or a lifetime.
Other Treatments for Dyspareunia (Surgery, Drugs)
Intercourse pain is an area that often confounds physicians and their patients. The tiny adhesions we have found to be the cause of pain are microscopic and do not appear in diagnostic tests. In addition, the delicate tissues of the vagina are not generally amenable to surgery, which itself can cause more adhesions. As a result, many gynecologists prescribe palliatives and pain relievers for patients who experience pain during or after sex. Typical gynecologic recommendations would be (in this order):
- Increase foreplay;
- Use more lubrication;
- If the above does not help, the doctor may prescribe either analgesics (pain relievers) or desensitizing gel (so the patient feels less pain). As a result, the patient is numbed to pain – and to pleasure;
- If the patient still has complaints of dyspareunia pain, she is generally referred to a psychologist or psychiatrist to help her deal with the pain issues. In some cases, the physician feels the pain is “all in the patient’s head.”
Published Research
To view a full list of success rates for treating painful intercourse and sexual dysfunction, please visit our Success Rates page.
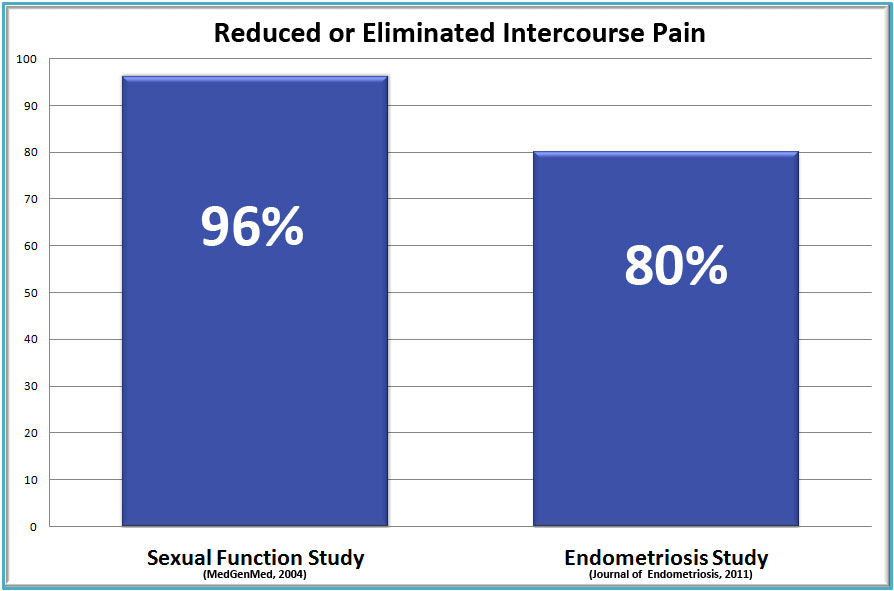
Our first sexual function study was published in Medscape General Medicine (Wurn et al., 2004b), a highly respected international medical journal owned by WebMD. In that study, our work decreased or eliminated intercourse pain in 96% of the participants. These published results represent one of our highest success rates among all of the conditions we treat. That same study reported improvements in every domain of sexual function for participants, including desire, arousal, lubrication, and orgasm. Subsequent study findings published in the Journal of Endometriosis investigated the decrease of painful intercourse in our patients with endometriosis.
In addition to eliminating intercourse pain, our therapy significantly increased orgasm and sexual function in our sexual function study participants (Wurn et al., 2011), as noted below:
- 64% reported increased intensity and duration of orgasm, or “first time in life” orgasms
- 71% reported increased desire (libido)
- 86% reported increased arousal
- 79% reported increased lubrication
- 71% reported increased satisfaction
- 94% reported decreased intercourse pain
- 93% reported improved overall sexual function
Testimonials
To read past patient success stories, please visit our Testimonials page.
Related Content:
- Intercourse Pain
- High Success Rates Treating Intercourse Pain, Naturally
- Three Common Causes of Deep Penetration Pain
- Sexual Health in Women Experiencing Sexual Pain: The Answer
- Causes of Decreased Sensation During Intercourse
- Overcoming Intercourse Pain: Reclaiming Desire and Orgasm
- You Don’t Have to Cope with Painful Intercourse While Trying to Conceive
If you’d like a free consult, please take 20 minutes and fill out this form and we can determine if therapy would be a good fit for you.